New Massachusetts General Hospital study on important heart issues in Lyme disease patients
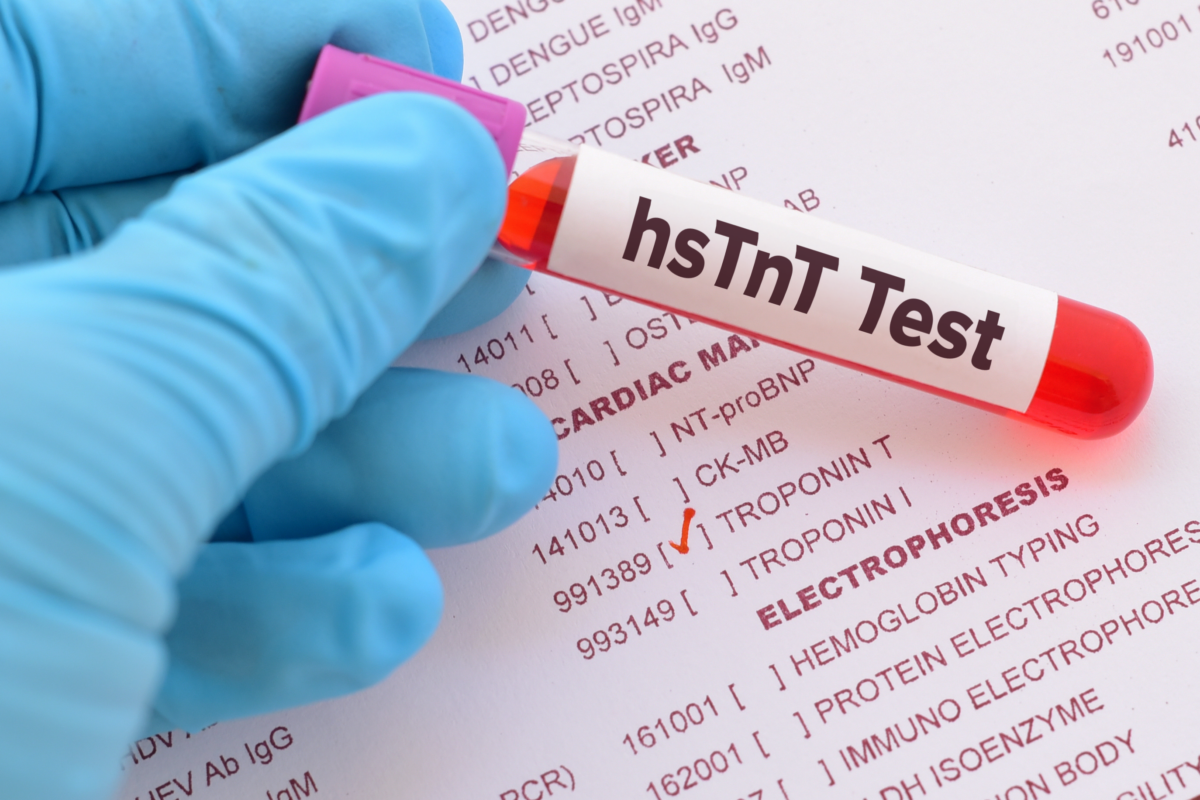
A Massachusetts General Hospital study that raises the awareness of possible cardiac involvement in early Lyme patients was recently published. This small study is the first to use data that measures a complex protein (troponin) to detect possible cardiac involvement in patients with early Lyme disease and with subclinical, or non-noticeable cardiac symptoms. Overall, 14.6% of the study subjects had elevated troponin T levels above the normal range. These findings were published in the March 2022 issue of Annals of Clinical & Laboratory Science and are explained in a new course from Invisible International, taught by first author Elizabeth Lee Lewandrowski, PhD, MPH, an Assistant Professor of Pathology at Harvard Medical School, a Faculty Researcher and Clinical Laboratory Scientist in Pathology at Massachusetts General Hospital, and Invisible International’s Research Director.
Troponin is a complex of three proteins (troponin T, I, and C) that regulate muscle contractions in the heart. When the heart is damaged, these proteins are released into the bloodstream, allowing clinicians to measure levels to determine the extent of heart damage. Both troponin T and I are detected and elevated in the blood when the heart is negatively impacted by various conditions, including infection, inflammation, or muscle damage. Therefore, this is potentially an important test for doctors to follow in the event of suspected cardiac involvement including subclinical cardiac involvement in patients with Lyme disease.
Previously, the Centers for Disease Control and Prevention reported that Lyme carditis occurs only in about 1% of Lyme disease cases (2008 to 2017). This newer study of 41 early Lyme patients used the high sensitivity troponin T test and found that 14.6% had elevated troponin T levels, suggesting that the heart is damaged in more early Lyme disease cases than previously realized. This finding should be brought to the attention of healthcare providers as it suggests cardiac involvement in early Lyme disease may be more common than previously realized. While there are many explanations for elevated troponin levels in these patients, including a systemic inflammatory response, this result raises the question that subclinical cardiac involvement may be more common than previously recognized. Further investigation is necessary to explore and validate the significance of this finding.
Some of the heart conditions that troponin T tests can detect include electrical disruptions (AV block, most common in Lyme carditis), inflammation (myocarditis), swelling of the heart sac (pericarditis), inflammation of the inner lining and valves (endocarditis), problems with the pumping action (cardiomyopathy), and heart attacks (myocardial infarctions). Some of these conditions can be fatal, emphasizing the need for rapid diagnosis and treatment when Lyme carditis is suspected.
The Invisible Education Initiative, funded by the Montecalvo Foundation, provides free, accredited Continuing Medical Education (CME) courses that focus on vector-borne and environmental illness within a One Health framework. These courses are available to clinicians and the public. To donate to this initiative and to learn about Invisible International, please go here http://invisible.international/give.