As 2022 comes to an end, the team at Invisible International is taking a moment to reflect on and celebrate our top five achievements of the last year. Invisible was founded only three years ago by a team of passionate and experienced physicians and scientists who recognized the need for a unique approach to solving the challenges of tick-borne illness. This dynamic team remains united around a common mission: To solve the persistent problem of vector- and tick-borne diseases with collaborative, creative educational approaches. In 2022, Invisible officially adopted the One Health framework, which positions its mission within the nexus of climate, human, and animal health. With this change, Invisible has many more collaborators and tools to engage new partners on the challenges of tick-borne disease. Invisible has a lot more in store for 2023, but let’s take a moment to celebrate the wins of 2022!
⁕ Our 30+ medical education courses had 7,000 views and received industry accreditation
The Invisible Education Initiative, funded by the Montecalvo Foundation, received accreditation from the prestigious Accreditation Council for Continuing Medical Education (ACCME) for its library of 30-plus continuing medical education courses. (Individual courses are accredited by the American Academy of Family Physicians.) These free courses serve up the latest in research and clinical advice on vector-borne illness, delivered by some of the most knowledgeable experts in their respective fields.
Why it matters: There’s a shortage of experienced tick-borne disease clinicians, with many patients having to wait months and travel long distances for appointments. Our free, on-demand courses—which have been viewed by 7,000+ health-care providers, medical schools, and patients—will increase the number of informed health-care providers. The education platform’s ACCME validation will encourage more physicians to take these courses for credit and will make it easier to integrate these courses into medical school curriculums. These courses will save lives.
⁕ Our storytelling team launched a Bartonella education campaign that reached millions
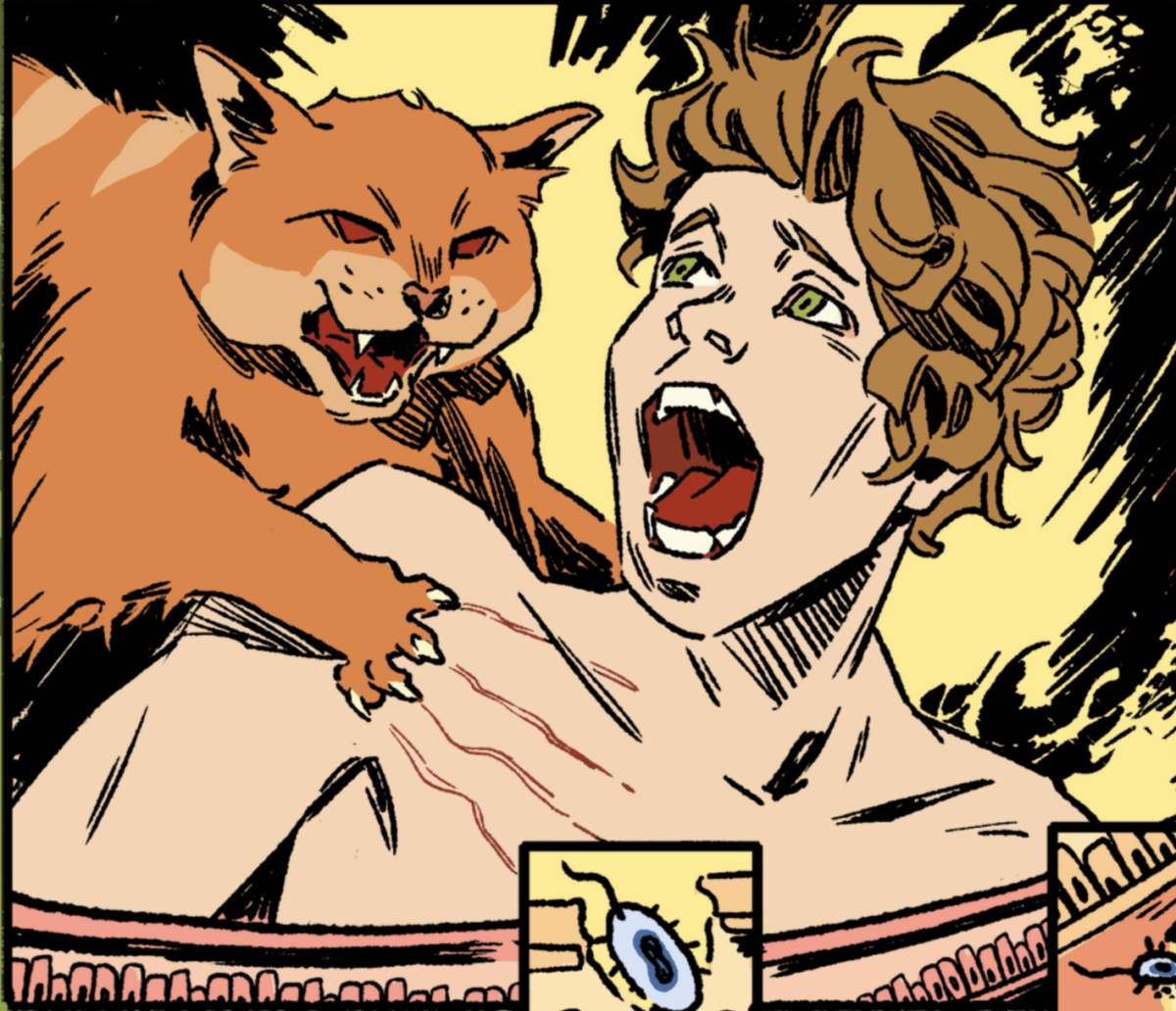
“Swamp Boy” — an article, video, and TikTok — tells the dramatic tale of a 14-year-old boy who suddenly experiences sudden-onset psychosis. The story follows his parent’s hellish journey into the medical system as they struggle to save their oldest son from permanent residency in a psychiatric ward. At the root of the teen’s medical problems was Bartonella henselae, a poorly understood stealth bacterium that causes cat scratch disease and disseminated Bartonellosis. This story was published through NowThis, which reaches 115+ million people and 60% of millennials (18-34) each month in the U.S. It was their #2 most read story in 2022 and was lauded by New York Times columnist Ross Douthat. The online story is backed up by a peer-reviewed case study and seven new medical education courses on Bartonellosis developed by members of our “Storytelling for Change” team.
Why it matters: This story is educating the public on common symptoms, testing strategies, and effective treatments for this misunderstood pathogen. It will help many sufferers shed the stigma associated with the mental health symptoms associated with these infections to seek treatment from Bartonella-aware physicians.
⁕ Our first “One Health” course is now featured on a CDC training website
Invisible is using the One Health problem-solving framework to reduce the impact of tick- and vector-borne diseases, which have worsened with climate change, ecosystem imbalances, and funding inequities. This year we released a new course taught by Cheryl Stroud, DVM, PhD, “One Health for Human Health Clinicians,” which helps clinicians view their most difficult patient diagnostic challenges through the eyes of a veterinarian and an academic researcher focused on environmental toxins. This course is featured on the CDC’s “Southeastern Center of Excellence in Vector Borne Diseases” training website.
Why it matters: The rise in vector-borne diseases is harming both humans and animals, yet veterinarians and physicians rarely share clinical wisdom on these common foes. Human clinicians can learn a lot from veterinarians on disease pattern recognition, diagnostic strategies, and prevention, and we’re trying to facilitate this transfer of knowledge through our courses.
⁕ Our online Hackathon brought global innovators together to propose solutions for connecting animal and human health experts
This year our Innovation Hackathon, funded by the Lovell Family Foundation, focused on enhancing communication between animal and human clinicians. During this One Health Day event, four winning teams received funding for proposals to develop 1) A social network for animal and human health professionals; 2) A comprehensive national review of childhood tick prevention education; 3) An AI-powered surveillance system for vector-borne diseases; 4) A novel tick-borne illness detection device
Why it matters: There are no easy ways for veterinarians, physicians, and public health officials from different countries to share emerging disease data and best practices. Yet diseases and epidemics don’t respect borders. We use our annual hackathons to encourage multidisciplinary teams from around the world to solve our toughest challenges in inventive, technology-driven ways.
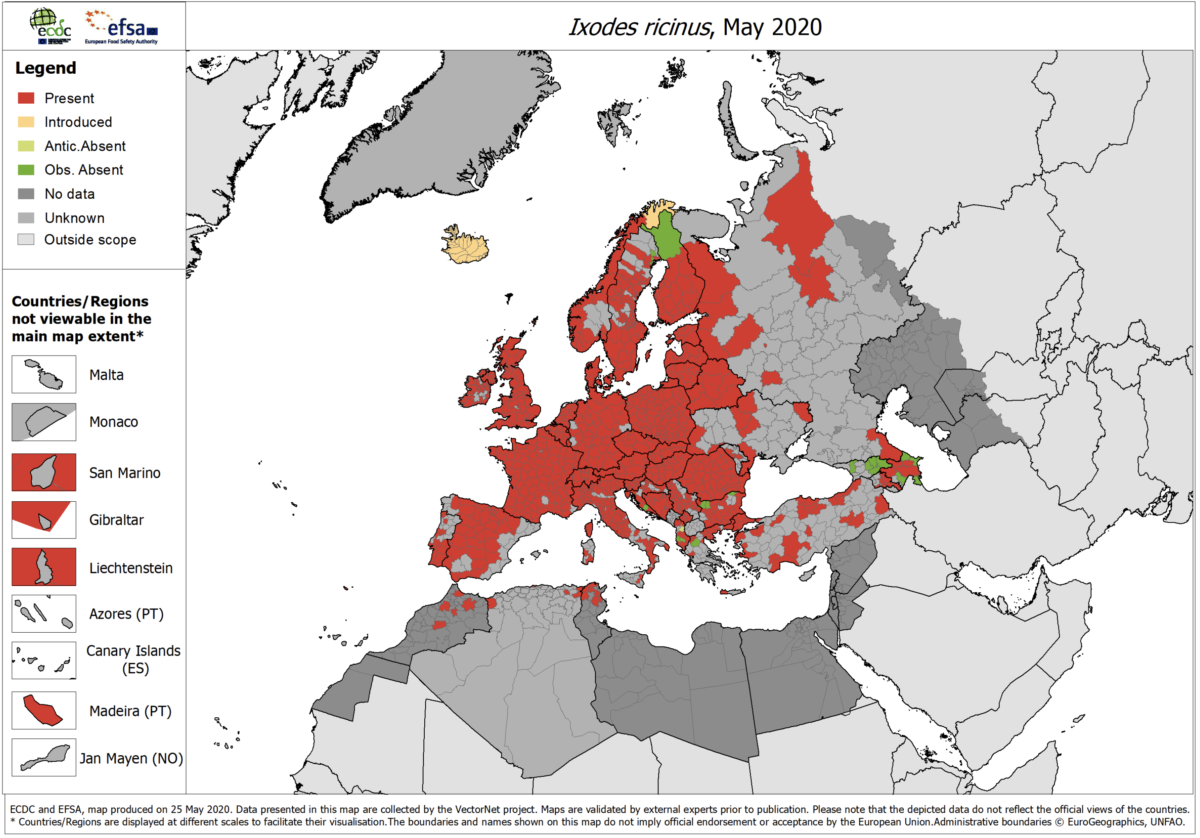
⁕ We expanded our educational partnerships to Europe and are sharing content with other Lyme nonprofits and wellness websites
This year our curriculum team added our first international CME instructor, Jack Lambert, MD, PhD, a Professor of Medicine and Infectious Diseases at Mater and Rotunda hospitals, a University College of Dublin School of Medicine in Dublin, Ireland, and the founder of the Lyme Resource Centre in Scotland. As we release new courses, our storytelling team works to maximize visibility through content-sharing with the Lyme community and popular wellness websites. For example, this year, MindBodyGreen and LymeDisease.org co-published two important articles on diagnosing tick-borne diseases in adults and young children, reaching millions.
Why this matters: The rise of tick-borne diseases is an international problem that is getting worse with climate change and global travel. After we invest in the development of evidence-based courses, we strive to share this information as widely as possible through strategic partnerships. We will continue to grow our international outreach in the coming year.
If you’d like to see more of these types of projects, please consider making a donation, no matter the size, to Invisible International. With your donation we will be able to continue to pursue medical education, research, and community empowerment programs, all with the mission of alleviating the suffering caused by invisible illnesses.
Wishing you all a healthy holiday and a prosperous new year. We know that our success wouldn’t be possible without your support, and we look forward to improving the health of all in the coming year.