The Power of Plants in Tick Prevention
As we embrace the beauty of spring and the outdoor activities it brings, we also face the increased risk of tick encounters. Read on to gain insights on how gardeners can use specific plants to protect themselves from ticks and the diseases they carry, such as Lyme disease—a condition that affects 476,000 Americans annually.
Q: Why is it important for gardeners to consider tick-repelling plants?
A: With tick-borne diseases on the rise, it’s crucial we utilize every tool in our arsenal for prevention. Tick-repelling plants are a natural, aesthetic way to make our gardens less hospitable to ticks and the wildlife that carries them. This method complements other preventive measures, creating safer outdoor spaces for everyone.
Q: Lavender is popular in gardens. How does it deter ticks?
A: Lavender’s lovely fragrance, appealing to humans, is detestable to ticks. Its beautiful blooms add color and fragrance to your garden while acting as a natural line of defense against ticks.
Q: Can you tell us more about how rosemary helps repel ticks?
A: Absolutely. Rosemary emits a strong aroma that ticks find repulsive. It’s an excellent choice for gardeners because it’s not only effective against ticks but also enhances your garden’s aroma and is useful in the kitchen. Plus, it’s drought-resistant, making it a low-maintenance option for busy gardeners.
Q: What makes wormwood a good addition to a tick-preventive garden?
A: Wormwood contains absinthin, a bitter compound that’s unappealing to both ticks and their common hosts, like deer and mice. Its silver foliage adds beauty to your garden while serving as a natural pest deterrent.
Q: How does garlic contribute to tick prevention?
A: Garlic’s strong scent is a natural pest repellent, including ticks. Planting garlic around your garden can create a barrier that ticks are likely to avoid. It’s also a bonus for gardeners who love cooking with fresh herbs.
Q: Mint is known for its invasiveness. Is it still worth planting for tick prevention?
A: While mint does require careful management to prevent it from taking over, its strong scent is highly effective at repelling ticks. I recommend planting mint in containers to keep it contained while leveraging its tick-repelling properties. It is also a wonderful culinary herb that makes for a healthy and flavorful addition to dishes, sauces, and drinks.
Q: Geraniums are beautiful but toxic to pets. How do they fit into tick prevention?
A: Geraniums contain geraniol, which is effective against ticks. However, their toxicity to pets means they should be used with caution. If you have pets, consider placing geraniums in areas your pets don’t access or choosing other plants from this list.
Q: Marigolds are bright and cheerful. Do they repel ticks?
A: Yes, marigolds emit a fragrance that ticks dislike. They’re easy to grow and can add a protective and colorful edge to your garden.
Q: Can you explain how chrysanthemums contribute to tick prevention?
A: Chrysanthemums contain pyrethrin, a natural insecticide that repels ticks. Incorporating these flowers into your garden can provide a natural defense against ticks while adding beauty to your landscape.
Q: Lemongrass is often associated with citronella. How does this plant help in repelling ticks?
A: Lemongrass contains citronella oil, which is a well-known insect repellent. Planting lemongrass can help keep ticks at bay, and it offers the added benefit of being a delicious culinary herb. Its tasty tea is research-proven to help fight off infections and reduce cholesterol.
Q: Any final thoughts or advice for our readers?
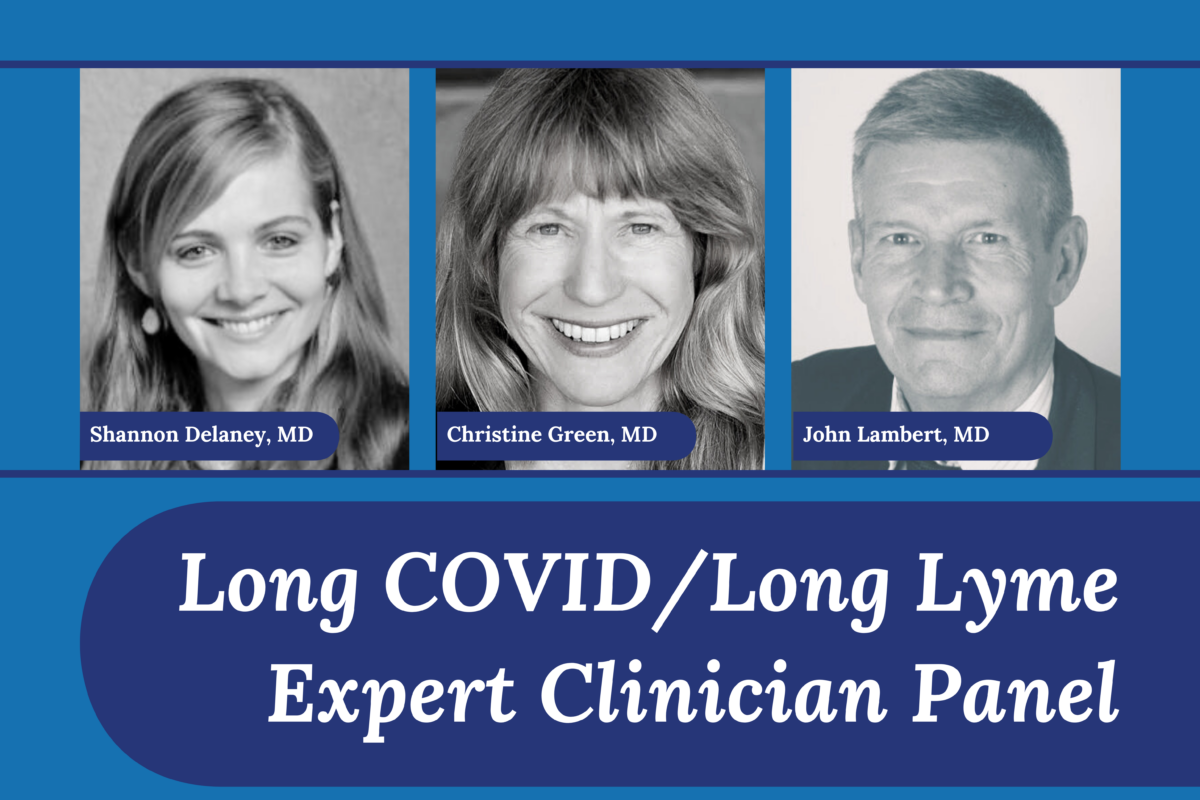
A: While incorporating tick-repelling plants is a powerful strategy, it’s important to approach tick prevention holistically. This includes regular yard maintenance, using personal repellents, and conducting tick checks after outdoor activities. Additionally, we encourage everyone to gain in-depth knowledge by accessing the free, accredited Continuing Medical Education (CME) courses on vector-borne and environmental illnesses offered by the Invisible Education Initiative, funded by the Montecalvo Foundation. These resources are invaluable for both clinicians and the public in understanding and combating tick-borne diseases.
For Further Reading and Resources:
- Centers for Disease Control and Prevention (CDC): Tick-borne Diseases
- Gardening Know How: Using Plants for Natural Pest Control
- Finally, don’t forget to do your tick checks!
By incorporating these tick-repelling plants into your garden, you can enjoy the outdoors with a little more peace of mind, knowing you’re taking steps to protect yourself and your loved ones from tick-borne illnesses.
Support Invisible International, a 501c3, and learn more about our educational programs.